Aortic intervention has attracted renewed interest since endovascular alternatives were introduced, which are distinct because of their minimally invasive nature. There is agreement today among the vascular community that an endovascular-first approach to aortic interventions should be taken, including endovascular aortic repair (EVAR), thoracic endovascular aortic repair (TEVAR) and transcatheter aortic valve implantation (TAVI).
Substantial improvement in 30-day mortality has been reported in several pivotal randomised controlled trials1–4 investigating EVAR instead of open surgery for abdominal aortic aneurysm (AAA). However, a matched propensity score analysis demonstrated that this advantage diminished in the long term, specifically after 3 years.5 This was also reflected in the meta-analysis of a recent Cochrane review, which found EVAR conferred no intermediate- and long-term mortality benefits.6 Similar observations were noted in the INSTEAD trial, where TEVAR failed to demonstrate improved overall survival for patients with uncomplicated type B aortic dissection.7 Nonetheless, both TEVAR and EVAR remain robust tools in the surgeon’s armamentarium, especially for patients considered unfit for conventional surgery.
Valve procedures have also witnessed a paradigm shift in the contemporary endovascular era. Patients with diseased valves traditionally underwent valve replacements during open surgery. However, open surgical repair started losing its traction ever since the inception of TAVI, which was pioneered by Cribier et al. in 2002.8 Since then, evidence has suggested that patients on the entire risk spectrum for valve degeneration benefit from TAVI, as demonstrated in a meta-analysis of patients at low and moderate risk,9 as well as in the PARTNER and PARTNER 1 trials that involved high-risk patients with aortic stenosis.10,11
However, these trials tend to include patients suitable for the conventional access routes, although some are contraindicated for these first-line options. The success of all three endovascular procedures conceivably depends on the technical difficulties of fitting a stent graft or aortic valve to the aorta. The femoral approach retains its ubiquitous appeal among vascular surgeons because of it is minimally invasive,12–14 and it has recently been agreed by the American College of Cardiology (ACC) expert consensus panel as the vessel of choice for TAVI procedures.15 However, an estimated 20 % of patients undergoing TAVI are not suitable for the transfemoral approach because the condition of the vessel makes this unfeasible. Similar observations have been made in patients undergoing EVAR, where 13 % of patients were deemed unsuitable for the transfemoral access, as reported in the European Collaborators on Stent-Graft Techniques for Abdominal Aortic Aneurysm Repair (EUROSTAR) registry.16
Despite the feasibility of alternate access techniques such as the transapical, transaortic and transaxillary17 routes, patients with previous coronary bypass artery grafts, respiratory pathology, porcelain aorta or inadequate vessel size would normally be excluded from these approaches. Therefore, some patients are precluded from open surgery and first-line as well as alternative vessel access routes. This quandary may have been resolved when May et al. pioneered the use of the carotid artery as an access option.18 Although it is regarded as last resort in the ACC guidelines15 as well as in modern practice,19 it offers a shorter and direct route to the aorta from the site of entry with improved movement stability and accuracy of catheter delivery.17,20
The following sections will examine the transcarotid approach with contemporary evidence, as an alternative or even potentially first-line access route for endovascular interventions of the aorta.
Transcarotid Endovascular Repair and Thoracic Endovascular Repair
Procedural Technicalities
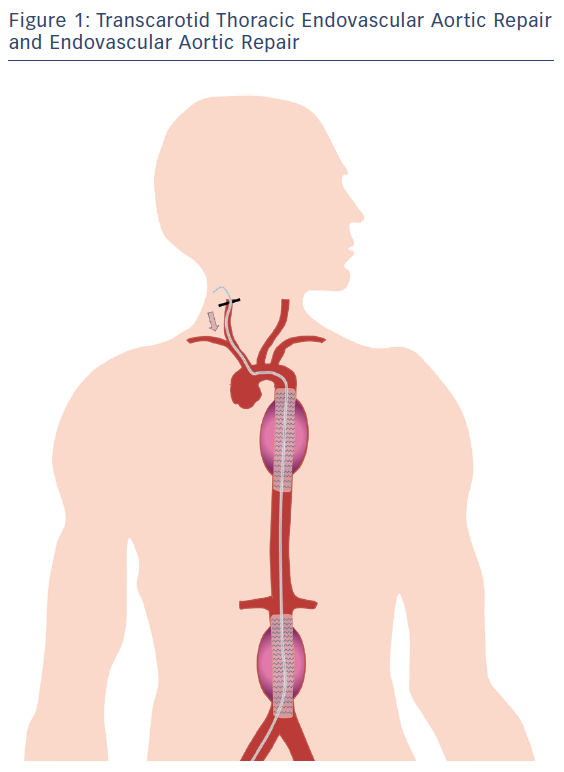
Figure 1 depicts an EVAR and a TEVAR performed via the carotid artery. Because of the relative infancy of the transcarotid method, there are inconsistencies in how the procedure is carried out. For instance, a range of preoperative investigations can be used to identify disease-free carotid arteries, including angiography, CT angiograms, angiography, MRI and transcranial Doppler. Once systemic anticoagulation has been administered, a low anterior neck incision will be made to expose either of the common carotid arteries. Typically, vessel access can be obtained using a 19-F gauge needle, followed by advancing a guidewire under fluoroscopic control into the aorta. A 5F pigtail catheter with 1 cm measurement markers is used to administer contrast to conduct an aortogram. An oblique arteriotomy is performed in the proximal common carotid artery to facilitate advancement of the endograft caudally over a flexible guidewire into the aorta.
Targeted measures can be employed to reduce the inadvertent risk of both proximal and distal attachment site migration, given presence of ‘windsock’ forces, particularly at the former. This includes augmenting the systemic blood pressure and administering adenosine to induce temporary asystole during deployment of the proximal attachment site. Finally, a balloon can be used to dilate both proximal and distal sites to achieve optimal fixation.20,21 Angiographies should be performed to ensure correct positioning before releasing the caudal and cranial trigger wires. In addition, surgical adjuncts should be considered to prevent complications. Clamping the distal common carotid artery may help to prevent catheter-associated embolisation.20,22,23 Carotid–carotid or carotid–carotid–subclavian bypasses can also be performed to increase intraoperative cerebral perfusion.24
Neurological Complications
There is, unsurprisingly, a lack of enthusiasm for the transcarotid approach in both EVAR and TEVAR, which is evident from the dearth of literature. The first reported case of transcarotid EVAR was in a patient who required a proximal Type 1 endoleak repair following a large AAA repair.18 As the patient had torturous iliac vessels and a small axillary artery, traditional access routes were rejected in favour of the right common carotid artery. This first case was successful and had no significant complications, providing novel insights into an untried method. Similar indications were observed in a separate case report of a patient with extensive calcific occlusive disease, which precluded him from the iliofemoral approach. Although there is an inherent risk of stroke from cerebral emboli or hypoperfusion, intraoperative surveillance by duplex ultrasound scanning or CT imaging allows for detection and prompt neurointervention. The risk of cerebral ischaemia associated with common carotid clamping is alleviated by collateral flow through the external carotid vasculature.
It is therefore imperative that both carotid arteries are disease free so the endograft can be accommodated and cerebral perfusion maintained.
Neurological complications – or any complications for that matter – could be more likely to occur in patients with thoracic arch pathologies, where unfavourable arch anatomies jeopardise the relative ease and safety of carotid access. This was highlighted in a case report by Heidenreich et al.,25 where a patient experienced multifocal infarct as a result of dislodged emboli during the process of traversing through a diseased aorta. Therefore, patients with unfavourable angulation of the left common carotid artery in relation to the aorta, aortic tortuosity or bovine anatomy25 should be identified with preoperative carotid duplex assessment.
A combination of the following factors could reduce the risk of neurological complications: anticoagulation therapy; multiple shorter devices instead of one longer device; and attaining an ideal angle of approach.
Much remains to be improved in terms of intraoperative monitoring, given the poor adoption rate of transcranial Doppler or stump pressure monitoring.24,26,27 One other tool to consider in future cases is cerebral oximetry, which is used in routine practice to monitor neurological changes during TAVI procedures.28
Other Complications
Apart from neurological complications, EVAR and TEVAR are often associated with delayed endoleaks; however, only two cases so far have been reported on this potentially calamitous complication.2,29 Although access site complications such as infection or haematoma are important site-specific issues, no studies so far have reported any occurrences of the aforementioned. Nonetheless, we recommend future studies to be consistent in reporting these clinically important complications.
Choice of Common Carotid Artery to Access
Another contentious issue is deciding which common carotid artery to access. Advocates of the right common carotid artery say it confers a more favourable angle of approach to the aortic arch,18 particularly for right-handed surgeons.20 However, this appears to hold true for the left common carotid artery as well, since it offers a straighter and more direct route to the descending aorta.25 Ultimately, choice depends on the diameter of the carotid artery itself, which is known to provide a large diameter entry site, although vessels tend to be larger in men than women.30 Given this, it is more important to make a choice based on prioritising larger-sized arteries with minimal occlusive disease over vessel site per se for successful deployment of the device, and this decision should be made on a case-by-case basis.
While the carotid artery has an advantage in having a wider diameter than other vessels, this may cease to be an issue in the light of technological advancements where newer devices with smaller sheath sizes could be the solution to the problems associated with smaller vessels.
Mortality
To date, the only case of mortality was reported by Faccenna et al.,26 where the patient experienced multi-organ failure stemming from acute pancreatitis. Because of the his past medical history of necrotising pancreatitis, the patient had a higher risk of organ ischaemia. In spite of that, it is erroneous to interpret the mortality rate for transcarotid EVAR and TEVAR at this present stage. Moreover, patients who undergo this procedure typically have numerous comorbidities, which is why they have been precluded from surgical or first-line vessel options. Publication bias in these studies could partially explain the relatively low and comparable mortality rate, as evident in the EVAR 2 trial where 30-day mortality rate was 7.3 %.2 In the light of this, the authors recommend future research that consider cohort studies with larger sample sizes to establish any firm conclusions.
Transcarotid Transcatheter Aortic Valve Implantation
Procedural Technicalities
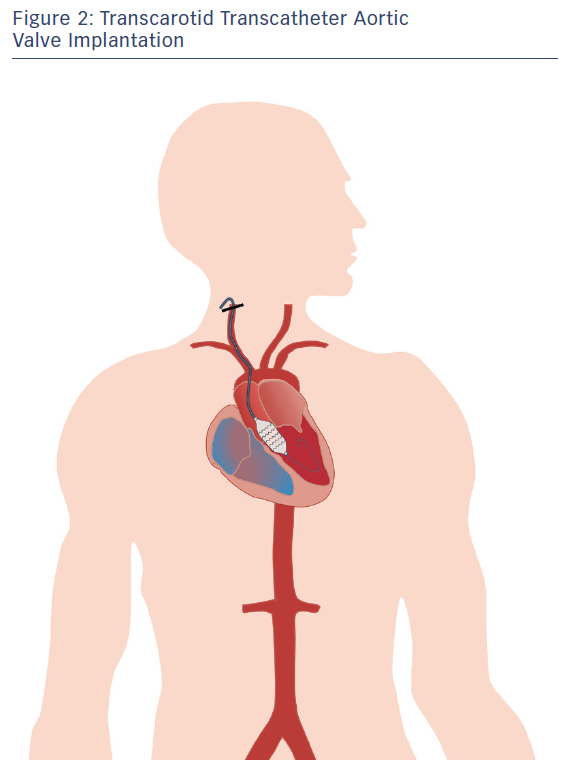
Figure 2 depicts TAVI performed via the carotid artery. The transcarotid approach for transcatheter aortic valve implantation remains an alternative approach when all other vessel or open surgery options have been rejected. Nonetheless, its adoption has been growing, as evident from the FRANCE-TAVI registry, which reported a 3.4 % proportion of transcarotid access.31
Before starting the procedure, it is essential to conduct a Doppler study and CT angiography of the carotid and vertebral vasculature to assess carotid patency, as well as of the Circle of Willis to evaluate the risk of cerebrovascular hypoperfusion.
The procedure is often performed in a hybrid operating theatre involving a multidisciplinary team of a vascular surgeon, interventional cardiologist, cardiac surgeon, anesthesiologist and radiology technician. Under general anesthesia, a vertical 2–3 cm incision can be made one or two fingers above the left clavicle to expose common carotid artery. The common carotid artery is then carefully dissected to avoid damaging the vagus nerve. To ensure catheter and sheath stability during intravascular navigation, another small incision 1 cm above the first incision can be made. To prolong activated clotting time to 250 seconds and beyond, intravenous heparin should be administered. Next, a 0.035-inch J-tipped soft guidewire can be employed to guide the pigtail catheter, followed by changing it to a straight-tip guidewire to cross the aortic valve. When finally pushed in to the left ventricle, the straight guidewire can be switched to a stiff guidewire. Thereafter, the valve system (CoreValve Evolut R, Edwards Sapien valves) can be loaded into the delivery system (EnVeo R, Medtronic), and their orientation checked. Once the catheter has progressed through the carotid artery and aorta, and properly positioned, the valve can be deployed without rapid pacing. It is important to assess for periprosthetic regurgitation using aortography before removing the carotid sheath. Once the procedure has been completed, the arterial access site can be sutured in a transversal fashion using PROLENE® sutures, with short clamping both proximally and distally to the access site.32–34
Mortality
Encouraging evidence for the transcarotid approach has emerged, and it has gradually been accepted as the alternate access route in patients who are contraindicated for the transfemoral route. This was discernible in a single centre where 137 TAVI procedures were conducted employing transfemoral, transapical and transcarotid approaches.19 The main finding was that in-hospital mortality rates between the transcarotid and transfemoral approaches were comparable. Furthermore, the former had a shorter procedural time and patients had a shorter overall length of stay in the intensive care unit. Because of these positive findings, the transcarotid approach has become be the choice of alternative access route for that centre.19 Similar findings were observed in a landmark study of 174 patients who underwent transcarotid TAVI in two French centres.35 Here, 30-day mortality was 7.4 %, which compares favourably with the transfemoral and transapical approaches demonstrated in recent meta-analyses.36,37 This was recently corroborated in a systematic review of real-world evidence, which reported a pooled mortality rate of 4.1 % across 16 studies.28
Risk of Neurological Complications
The risk of neurological complications, including ischaemic stroke and transient ischaemic attacks (TIAs) are the Achilles’ heel of this approach. However, registry data has been reassuring, and shows that preoperative imaging is critical to preventing cerebrovascular events. For instance, the in-hospital stroke rate was reported to be only 2 % in the FRANCE TAVI registry.31
Surgical adjuncts remain contentious. Carotid bypass or shunting have been advocated to maintain intraoperative cerebral perfusion38,39 but these compromise procedural time and increase the risk of complications.19 Instead, comprehensive preoperative evaluation has been espoused as the strategy of choice to monitor cerebral perfusion, as evident from the French Transcarotid TAVI Registry.34 Furthermore, concerns about distal carotid clamping were assuaged when Kirker et al. demonstrated the absence of in-hospital neurological complications arising from the procedure. This, however, required scrupulous attention to reduce occlusion time coupled with intraoperative monitoring of cerebral oxygen saturation using cerebral oximetry.19 The success of these techniques was bolstered by another group, which performed transcarotid TAVI on five patients, none of whom experienced cerebrovascular complications.40 Cerebral oximetry has long been established as a useful adjunct in carotid endarterectomy,41 and is likely to remain as the cornerstone of neurological monitoring in transluminal procedures involving the carotid artery. Clinical monitoring of the neurological status during a transient carotid artery cross-clamping test (awake testing), is an effective and simple method that should not be disregarded. Azmoun et al. champion awake testing as the optimum approach, even though it is limited to procedures performed under local anaesthesia. Furthermore, a temporary carotid shunt can be performed to potentiate passive antegrade carotid perfusion if the patient becomes intolerant to the cross-clamping test.42 The risk of stroke should not be taken lightly in spite of the relatively low incidence.43–45 Clinical trials have shown that the use of a cerebral protection device in patients with severe aortic stenosis undergoing TAVI reduced the risk of ischaemic cerebral lesions; however, adequately powered studies are still warranted to evaluate the efficacy of protection devices on neurological and cognitive function after a TAVI procedure.46 Until such devices are commercially available, technical modifications can be employed to abate the risk of debris entry into the brain. One such technique involves clamping the distal carotid artery with back-bleeding after successful deployment of the valve.19
Choice of Anaesthesia
Another unresolved issue involves the type of anaesthetic procedure. The use of general anaesthesia (GA) has risks of obstructive sleep apnoea, aspiration and hypotonic hypopharyngeal muscles, all of which are potentially fatal complications in a typical TAVI patient, most of whom are elderly.47 However, these do not explain the occurrence of perioperative stroke. In addition, GA prohibits real-time monitoring of neurological status, leading to prolonged cerebral hypoperfusion.41
The use of local anaesthesia (LA) permits awake testing during carotid cross-clamping, which is believed by some to be more robust for conducting neurological assessment.42 Furthermore, cross-clamping engenders an increase in systemic blood pressure and consequent cerebral perfusion.48
Despite the theoretical and hypothetical differences between GA and LA, the largest randomised controlled trial to date that compared LA with GA (the GALA trial) in carotid endarterectomy reported no significant differences in the risk of perioperative stroke.49 This was supported by a Cochrane review that included a meta-analysis of pooled data from 14 trials;50 however, 75 % of all patients in the review were part of the GALA trial.49
Paucity of Evidence to Date
The benefits of transcarotid TAVI have been well encapsulated in a systematic review28 and in a recently updated version.51 Although the pooled data suggest that the carotid artery may be a viable alternative, the overall quality of data is poor because of the paucity of RCTs. Selection bias is inherent and inevitable, since most patients included were already precluded from open surgery, transfemoral or transapical TAVIs because of unfavourable baseline characteristics. Despite the unmet need for future research to conduct RCTs, we recognise it may never be possible to perform a proper RCT given ethical considerations.
Conclusion
The emergence of encouraging results has led to the adoption of the transcarotid approach for aortic interventions as an alternative access route for patients who are contraindicated for the transfemoral approach.
However, technical details remain to be ironed out, including those of choice of anaesthesia, whether to use the left or right carotid artery and approaches to neurological monitoring. Given a large and proper RCT comparing transcarotid against transfemoral approaches is unlikely to be conducted, the authors cannot draw any firm conclusions from the current pool of literature. While recent retrospective cohort studies have encouragingly shown similar levels of safety and efficacy between transcarotid and transfemoral TAVI approaches,52,53 this must be interpreted in the context of known limitations, such as selection and confounding biases.
In this light of this, it is inconceivable for prospective guidelines to recommend the carotid artery as the vessel of choice. The authors recommend future research that will consider cohort studies with large sample sizes. As to whether carotid access for aortic interventions is a “genius” or “madness”, judicious selection of patients on a case-by-case basis remains the most appropriate answer to this question. Current evidence does not allow us to conclude otherwise.